Statistical Issues in the Acupuncture for C-Section Study
/We need non-pharmacologic pain control options after c-section, but this acupuncture study has some concerning red flags.
Read MoreThe Risks of COVID-19 In Pregnancy
/Most births are uncomplicated, but coronavirus still increases the risk of bad outcomes dramatically.
Read MoreGastric Bypass May Reduce the Risk of Birth Defects
/A Swedish population-based study found that, despite concerns of folate deficiency, gastric bypass reduced the risk of major birth defects.
Read MoreSocial Media: the Future of Diagnosis?
/A study suggests that your Facebook posts can be used to determine what diseases or conditions you have with reasonable accuracy.
Read MoreIntervention to Increase Monitoring of Fetal Movements Not Helpful, Maybe Harmful
/A large, randomized trial in the UK found that encouraging women to track their baby’s movements did not reduce stillbirth rates.
Read MoreAcupuncture Provides No Benefit During In Vitro Fertilization - In Fact, It Might Be Harmful
/A new study shows that acupuncture is no more effective than sham acupuncture for women undergoing IVF. That means it doesn't work. Sort of.
Read MoreGut Bacteria May Link Maternal, Child Weight
/Overweight mothers tend to have overweight children, but the link is not entirely genetic. A new study suggests that the gut microbiome may play an important role.
Read MoreBirth at 41 Weeks = Baby Genius?
/A study appearing in JAMA Pediatrics suggests that children born late-term have better cognitive outcomes than children born full-term. As if pregnant women didn’t have enough to worry about. For the video version of this post, click here.
Let’s dig into the data a bit, but first some terms (sorry for the pun). “Early term” means birth at 37 or 38 weeks gestation, “full term” 39 or 40 weeks, and “late term” 41 weeks. In other words, this study is not looking at pre-term or post-term babies, all of the children here were born in a normal range.
Ok, here’s how the study was done. Researchers used birth records from the state of Florida and linked them to standardized test performance in grades 3 through 10. Compared to children born at 39 or 40 weeks of gestation, those born at 41 weeks got test scores that were, on average, about 5% of a standard deviation higher. To get a sense of what the means, if these were IQ tests (they weren’t) that would translate to a little less than 1 IQ point difference. Not huge, but the sample size of over one million births makes it statistically significant.
10.3% of those born at 41 weeks were designated as “gifted” in school, compared to 10.0% of those born at full-term.
Before I look at what might go wrong in a study like this – is the effect plausible? To be honest, I sort of doubt it. One week extra development in utero certainly will lead to some differences at or near birth, but I find it hard to believe that any intelligence signal wouldn’t simply be washed away amid all the other factors that affect developing young minds prior to age 8.
Now, the authors did their best to adjust for some of these things – race, sex, socioeconomic status, birth order, but it seems likely that there are unmeasured factors here that might lead to longer gestation and better cognitive outcomes – maternal nutrition comes to mind, for example.
We also need to worry about systematic measurement error. These gestation times came from birth certificate data – in other words, many of these measurements may have been some doctors best guess. If the dates were determined by ultrasound, larger babies might be misclassified as later term. Also, I suspect that if conception dates weren’t well known, a lot of doctors filling out the birth certificate may have just written “40 weeks” to put something in that box.
The authors attempted to look just at women where the likelihood of prenatal care was high, finding similar results, but again, with the tiny effect size, any small systematic measurement error could lead to results like this.
The authors state that this information is relevant to women who are considering a planned cesarean or induction of labor. Currently, the American College of Obstetrics and Gynecology recommends “targeting” labor to 39-40 weeks to avoid some physical complications of late-term birth. In my opinion, having this study change that recommendation at all would be premature.
Pregnancy, Multiple Sclerosis, and Vitamin D: The Latest Hype
/A study appearing in JAMA neurology links better Vitamin D level in pregnant women to a lower risk of multiple sclerosis in their offspring. There are some really impressive features of this study, but there are some equally impressive logical leaps that seem to defy the force of epidemiologic gravity. Let's give the study some sunlight.
For the video version of this post, click here.
The study was run out of Finland, which is a country that figured it might be a good idea to keep track of the health of its citizens. In fact, since 1983, nearly every pregnant woman in Finland has been registered, and a blood sample sent to a deep freezer in a national biobank. The researchers identified 193 individuals with MS, and went back into that biobank to measure their moms' vitamin D levels during pregnancy. They did the same thing with 326 controls who were matched on their date of birth, mother's age, and region of Finland.
This is from the first line of their discussion:
Wow. 90%. That sounds scary. And the news outlets seem to think it is scary too. But that impressive result hides a lot of statistical skullduggery.
Here's the thing, Vitamin D level is what we call a continuous variable. Your level can be 5, 10, 17, 42, whatever – any number within a typical range. When you study a continuous variable, you have to make some decisions. Should you chop up the variable into categories that others have defined (like deficient, insufficient, normal), or should you chop it up into even-sized groups? Or should you not chop it up at all?
As a general rule, you have the most power to see an effect when you don't chop at all. Breaking a continuous variable into groups loses information.
When the Vitamin D level was treated as the continuous variable it is, there was no significant relationship between Vitamin D level in mom and MS in the child. When the researchers chopped it into 5 groups, no group showed a significantly higher risk of MS compared to the group with the highest level. Only when they chopped the data into 3 groups did they find that mom's who were vitamin D deficient had 1.9 times the risk of those that were insufficient. That's the 90% figure, but the confidence interval ran from 20% to 300%.
And did I mention there was no accounting for mothers BMI, smoking, activity level, genetic factors, sun exposure or income in any of these models? Despite that, the paper's conclusion states :
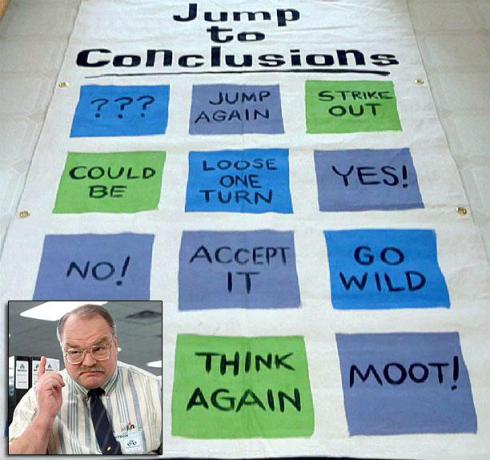
That statement should go right on the jump to conclusions mat.
Look, I'm not hating on Vitamin D. I actually think it's good for you. But research that adds more to the hype and less to the knowledge is most definitely not.