Pregnancy, Multiple Sclerosis, and Vitamin D: The Latest Hype
/A study appearing in JAMA neurology links better Vitamin D level in pregnant women to a lower risk of multiple sclerosis in their offspring. There are some really impressive features of this study, but there are some equally impressive logical leaps that seem to defy the force of epidemiologic gravity. Let's give the study some sunlight.
For the video version of this post, click here.
The study was run out of Finland, which is a country that figured it might be a good idea to keep track of the health of its citizens. In fact, since 1983, nearly every pregnant woman in Finland has been registered, and a blood sample sent to a deep freezer in a national biobank. The researchers identified 193 individuals with MS, and went back into that biobank to measure their moms' vitamin D levels during pregnancy. They did the same thing with 326 controls who were matched on their date of birth, mother's age, and region of Finland.
This is from the first line of their discussion:
Wow. 90%. That sounds scary. And the news outlets seem to think it is scary too. But that impressive result hides a lot of statistical skullduggery.
Here's the thing, Vitamin D level is what we call a continuous variable. Your level can be 5, 10, 17, 42, whatever – any number within a typical range. When you study a continuous variable, you have to make some decisions. Should you chop up the variable into categories that others have defined (like deficient, insufficient, normal), or should you chop it up into even-sized groups? Or should you not chop it up at all?
As a general rule, you have the most power to see an effect when you don't chop at all. Breaking a continuous variable into groups loses information.
When the Vitamin D level was treated as the continuous variable it is, there was no significant relationship between Vitamin D level in mom and MS in the child. When the researchers chopped it into 5 groups, no group showed a significantly higher risk of MS compared to the group with the highest level. Only when they chopped the data into 3 groups did they find that mom's who were vitamin D deficient had 1.9 times the risk of those that were insufficient. That's the 90% figure, but the confidence interval ran from 20% to 300%.
And did I mention there was no accounting for mothers BMI, smoking, activity level, genetic factors, sun exposure or income in any of these models? Despite that, the paper's conclusion states :
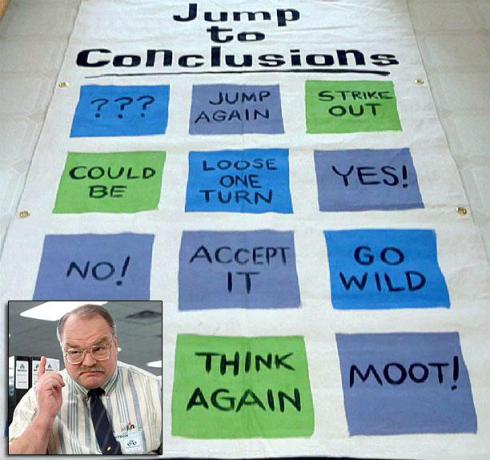
That statement should go right on the jump to conclusions mat.
Look, I'm not hating on Vitamin D. I actually think it's good for you. But research that adds more to the hype and less to the knowledge is most definitely not.
"Association" is a biomedical weasel-word. Does low Vitamin D cause MS?
/For the video version of this post, click here. Ill admit Im a bit of a vitamin D skeptic. Studies demonstrating that the wonder-vitamin can improve cognition, decrease the risk of colon cancer, and prevent heart disease are often observational in nature. These associations are always confounded by sunlight exposure and diet two factors which themselves are strongly associated with a variety of health outcomes. It's no surprise that randomized trials of vitamin D supplementation have been less than impressive.
So a study, appearing in PLOS medicine, linking lower Vitamin D levels to the development of multiple sclerosis caught my eye.
It has long been noted that MS is more common in latitudes further away from the equator, where people get less sun. It has also been shown that people with MS have lower Vitamin D levels than people without MS. In this analysis, the issues of confounding of Vitamin D levels is addressed via Mendelian randomization. Heres a thirty second primer:
You want to know if some biomarker (like vitamin D level) is causally linked to a disease (like MS). Vitamin D level is determined by a slew of things that you have no control over, like sun exposure, but there may be genetic polymorphisms that predispose you to lower-than-average vitamin D levels for your entire life. At birth, you may be "randomized" to one of these genes. If low vitamin D causes MS, than surely people who inherited those low-vitamin D genes would have a higher risk of MS.
The caveat is that those genes have to be linked to MS only through a Vitamin D pathway you want to avoid what's called "pleiotropy". And those genes need to not be near any other genes on the chromosome that can cause MS. Finally, the genes need to be randomly spread through the population of interest if they are preferentially carried by a certain ethnic group you might be finding a marker of increased risk in that group due to cultural, environmental, or other biologic factors.
Point is Mendelian randomization is hard. Did the authors make the grade?
First they identified 4 single-nucleotide polymorphisms (SNPs) that were associated with low Vitamin D levels from a database of over 30,000 individuals. These variants were all in genes related to Vitamin D synthesis or metabolism. They then looked for these SNPs in a huge genetic study of MS patients comprising 14,000 cases and 24,000 controls.
The big finding is that, yes, people with MS were more likely to carry at least one of those low vitamin D genes. And while the genes weren't obviously associated with MS risk factors outside of Vitamin D, they were involved in things like steroid synthesis, so the potential for unknown off-target effects is pretty high.
Best we can tell, the implication is that increasing your vitamin D level significantly by say 10 50 nmol/L may decrease your risk of MS by up to 50%. Clearly, these numbers will have to be borne out in clinical trials. But considering that genetically low vitamin D is a lifetime risk, my hope that a short-term vitamin D supplementation trial will show a positive effect is very slim. There are ongoing efforts to start a Vitamin D trial among individuals with a first MS flare but that is clearly not the population who was studied here.
In the end, this study ends up being long on methods, and short on actionable results.