Rapid Treatment of Children with Sepsis Saves Lives
/A study in the Journal of the American Medical Association Vindicates a Family Who Lost a Loved One to Sepsis.
Read More5-days of Antibiotics Won't Cut it for Middle Ear Infections
/A randomized trial appearing in the New England Journal of Medicine has shown with fairly compelling evidence that 5-days of antibiotic treatment isn't enough for little ones with ear infections. For the video version, click here.
Read MoreProbiotics, Asthma and Antibiotics: Too Pragmatic?
/A study appearing in the Annals of Family Medicine had disappointing news for individuals who were hoping for a "natural" way to help treat their asthma. But as my grandmother used to say "don't let a poorly designed trial substitute for a negative one". For the video version click here.
Read MoreWill antibiotics make our kids fat? Nope.
/For the video version of this post, click here. The ubiquitous and often inappropriate use of antibiotics is a serious public health problem. So is obesity. That these two factors could be linked is the conclusion suggested by a paper, appearing in the International Journal of Obesity, which leveraged the huge Geisinger health system database to examine the BMIs of children who had different exposures to antibiotics.
The researchers examined the records of just under 150,000 children ranging in age from 2 to 18 who had BMI measurements in the system. Now, the relationship between antibiotic use and BMI is complex, so they tried to characterize a couple of metrics. They examined the immediate effect of the antibiotic - how much BMI increase could be expected after exposure to antibiotics in the past year, but they also measured the persistent effect of antibiotics - how much BMI increase would be associated with your lifetime exposure to antibiotics.
In both cases, antibiotics were associated with higher BMIs, but numbers matter. Let’s start with the basics. 59% of the children in the cohort had at least one antibiotic prescription. Shockingly (to me at least), of the kids that had contact with Geisinger in their first year of life, 49% had an antibiotic prescription in that year. We prescribe a LOT of antibiotics.
As to the effects, the short-term effect was relatively modest. Kids who got antibiotics in the past year had a BMI about 0.05 points higher than those who didn’t. The cumulative effect was even smaller - about 0.01 BMI points for one prior antibiotic at any point in life, but more courses led to more BMI gain. Those who had seven or more courses of antibiotics had a BMI about 0.1 points higher than those who never got antibiotics. All of these associations were statistically significant, but this was a huge study - these changes in BMI don’t strike me as clinically meaningful.
Moreover, these children were not randomized to get antibiotics. The researchers adjusted for age, sex, race, and medical assistance, but that’s it. Socioeconomic status could play a major role here, and medical assistance is not a close enough proxy for that. I also wonder about secondhand smoke exposure.
Putting it all together, the great obesity epidemic can’t be tied to antibiotic use. In fact, these small effect sizes make me less worried about the effects antibiotics have on our children's weight.
That said, this is one case where I’m glad there is some media hype around the study. While the headlines warning that antibiotics are making your children fat are completely overblown, perhaps the negative press will reduce the over-prescribing of antibiotics. And that’s good, not because it will cure the obesity epidemic, but because it will impact the emerging epidemic of microbial resistance.
Have we been giving kids juvenile idiopathic arthritis inadvertently?
/For the video version of this post, click here. If youve ever taken care of a kid with juvenile idiopathic arthritis, it sticks with you. This disease, which is occasionally referred to as juvenile rheumatoid arthritis, isnt fatal, but it can rob children of the ability to be active, play, and grow - the real essence of childhood. And to date, we still dont know what causes it. Its clearly auto-immune, but there isnt even a serologic test for the disease.
An article appearing in Pediatrics, from Daniel Horton, and - full disclosure - several of my former Penn colleagues - links antibiotic exposure in childhood to the subsequent development of JIA.
The researchers used the huge Health Improvement Network dataset, which captures much of the primary care activities that go on in the United Kingdom. Examining over 140,000 children, they found 152 cases of JIA, and matched them based on age and gender to 10 controls each. The bottom line? 88% of cases had been exposed to antibiotics. 75% of controls had been exposed.
Of course, you get antibiotics for infections. And cases were more likely to have infections as well: 93% versus 85%. A question and an observation, then. Question: is it the infection that causes the JIA and the antibiotics are just a bystander? Observation: man, we give a lot of antibiotics to kids.
The authors did a tremendous job putting the blame on antibiotics here. With multivariable adjustment, infection fell away as a risk factor - antibiotics persisted. There was a dose-response finding as well - more antibiotic courses were associated with higher risk. There was also a temporal component - there was a higher risk of JIA if antibiotics were given within a year of the index date compared to earlier time points. Finally, they tried to rule out reverse causation by considering the diagnosis of JIA whenever the first symptom (like limp or joint pain) appeared.
Bottom line? I believe that this finding is real. Whether the offered explanation - that antibiotics affect the intestinal microflora and alter immunity - is true remains to be seen, of course.
But I want to use this study to illustrate one issue that plagues almost every study of risk factors - and that is a failure to give us a sense of the attributable risk. In other words - how many of the cases of JIA can be explained by antibiotic use, compared to other possible risk factors (like the things that went into the multivariable adjustment)? Can every case of JIA be traced back to some antibiotic exposure? Of course not - but how much of the variation is explained by this variable. Thats the information we need to actually counsel our patients.
One thing this study does is open the door to future research. Given the microflora argument, that research will likely involve a lot of stool collections. And that, my friends, is why Im occasionally glad that Im a nephrologist.
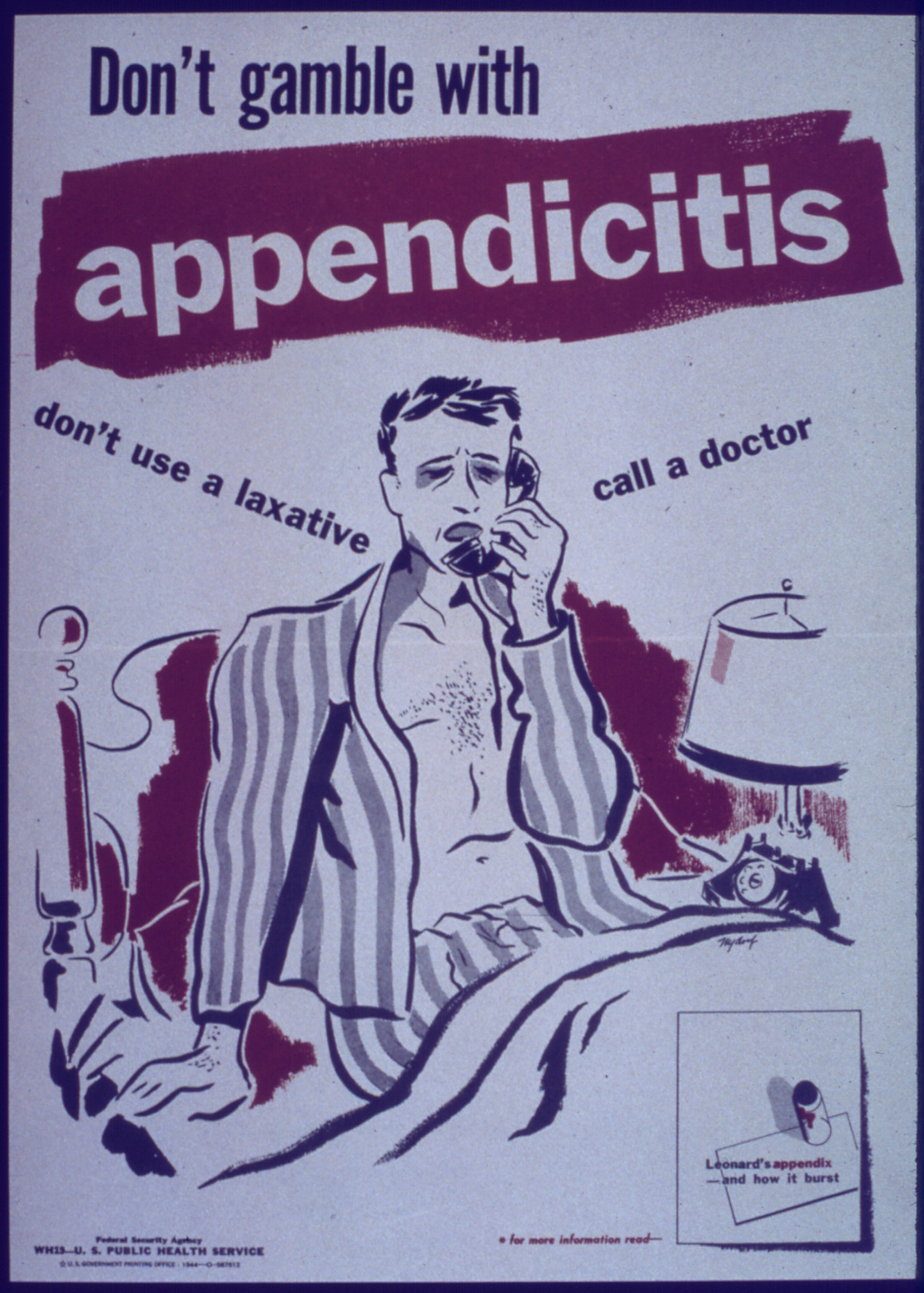
You operate on appendicitis, right? Right?!
/ For the video version of this post, click here.
For the video version of this post, click here.
If Greys Anatomy has taught us anything, its that you have to operate on appendicitis. This fact is imbued in the cultural zeitgeist - its the first book of the Madeline series for crying out loud. But paradigms, even one as inertial as this one, can shift.
Appearing in the Journal of the American Medical Association, a clinical trial attempted to show that, for appendicitis, antibiotic treatment alone may be no worse than a surgical approach.
Finnish researchers, led by Paulina Salminen, took 530 individuals with uncomplicated appendicitis (no perforation or appendicolith, basically), and randomized them to go to the operating room, or to get antibiotics instead: 3 doses of ertapenem (a broad-spectrum, IV antibiotic) followed by a week of oral levofloxacin and flagyl. After about a year of follow-up, the big question was how many people in the antibiotic group would have had to undergo surgery.
Of the 257 patients in the antibiotic group, 15 got operated on during the initial hospital stay. Another 40 would be operated on within the following year, a total of roughly 27% of the group. This missed the pre-specified non-inferiority target, but there are still some interesting numbers to look at.
First of all, lets consider why there was a surgical group at all. The only reason, really, is to look at the complication rate so we can see what antibiotics might help us avoid. Of the 273 people in the surgical group, 20% had complications, about half of which were surgical site infections and the remainder were due to pain and abdominal complications. Surgery has risk - and avoiding those risks, even in just 73% of cases, might be worthwhile.
But major caveat here: Almost all of these appendectomies were performed using an open technique, not laparoscopically. This is sort of crazy. Laparoscopic appendectomies lead to fewer infections, fewer abdominal complications, and a shorter length of stay. In speaking with some surgeons, I was told that the only reason theyd consider an open technique is for cases of complicated appendicitis, cases which were specifically excluded from this trial.
The authors write that they encouraged open appendectomies since resource-poor areas of the world might not have laparoscopic equipment, but this really ends up stacking the deck against surgery. If I were given the choice of a quick laparoscopic appendectomy with guaranteed results versus a 25% recurrence rate with antibiotics, I might take the surgery. But if my only choice was open surgery - with a risk of adhesions, obstruction, infection - well, antibiotics might just make the cut.
Fusobacterium necrophorum may be responsible for more cases of sore throat than Strep - and there's no test for it.
/ In this video, I discuss a recent article appearing in the Annals of Internal Medicine that documents an emerging bacterial cause of sore throat. But should we treat it aggressively?
In this video, I discuss a recent article appearing in the Annals of Internal Medicine that documents an emerging bacterial cause of sore throat. But should we treat it aggressively?
Check out my video commentary:
New Sore Throat Player, but There's a Catch | Medpage Today.






