1 of 9 American Men Have Oral HPV Infection
/A study appearing in Annals of Internal Medicine links infection to prior oral sex partners, among other risks.
For the video version, click here.
Human Papilloma Virus, the highly prevalent sexually transmitted infection, is like Amtrak on Thanksgiving - it comes with a lot of baggage. We associate HPV with cervical cancer, but somewhere between 2008 and 2012, oropharyngeal cancer overtook cervical cancer as the most common HPV-associated malignancy.
We used to associate oropharyngeal cancer with smoking, but the epidemiology demonstrates that in the modern era oropharyngeal cancer is really driven by HPV.
We consider HPV a disease with implications more for women than for men. This conception is also changing rapidly. While the rate of HPV-associated cancers are a bit higher in women than men, it's pretty close, and men have dramatically higher rates of oropharyngeal cancer due to HPV.
This is fascinating epidemiology, but we need more information on the mechanism. To begin to uncover what is going on with oral HPV, we are looking at this article, appearing in the Annals of Internal Medicine.
What we have here is a cross-sectional study looking at data from the National Health and Nutrition Examination Survey (NHANES to you and me). This is a representative survey of the US population at a single point in time.
Researchers took oral rinses to assess for HPV in nearly 10,000 individuals. They also asked a broad variety of questions about lifestyle and sexual history.
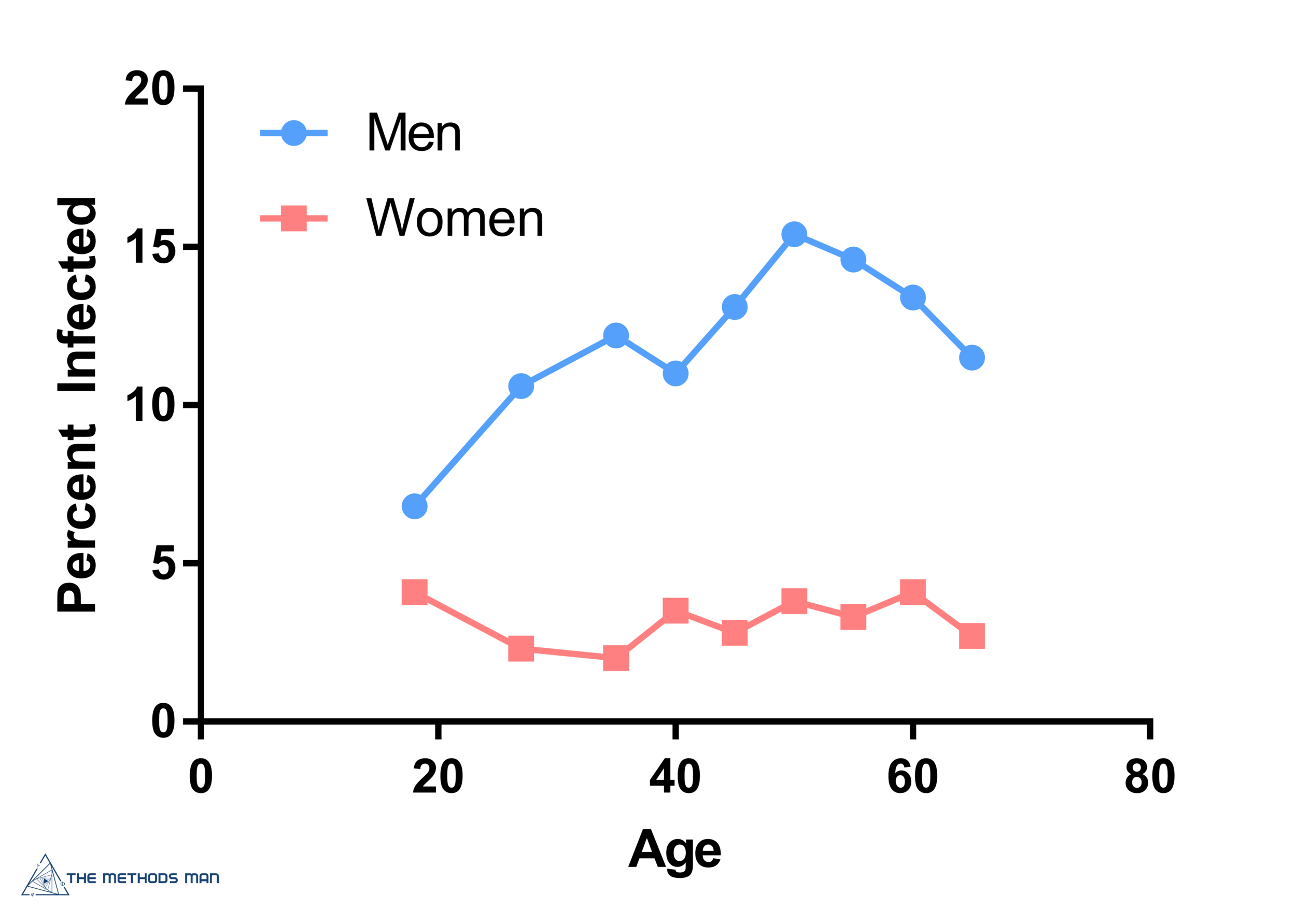
About 1 in 9 men had oral HPV infection, compared to 1 in 30 women. So, yeah, think about that when you kiss your loved one goodnight.
Furthermore, 63% of the infections in men were high-risk genotypes, compared to 44% in women.
The prevalence of infection in men climbed with age, peaking around age 50, while it remained relatively flat in the women.
What’s driving this in men? The link to certain sexual behaviors seems to be pretty clear. Infection is more common the more sexual partners and oral sex partners the men reported, both over the lifetime and in the past 12 months. But despite a certain voyeuristic interest, these data don’t seem highly relevant to me – changing sexual behavior is just not practical. Or fun.
What we can do is vaccinate. Now, in this cohort, HPV-vaccination was not associated with lower overall infection rates in either men or women, as you can see here.
But it was associated with lower infection rates with the four genotypes for which the vaccine provides protection suggesting that broader adoption of vaccination, particularly in men and boys, may be a reasonable policy.
The major issue with the study is its cross-sectional nature. We know that HPV infections can resolve spontaneously, can re-occur, may get passed between sexual partners repeatedly. A longitudinal study with detailed sexual partner analysis may be out of reach for practical purposes, but as the Bard said, “The course of true love never did run smooth”.